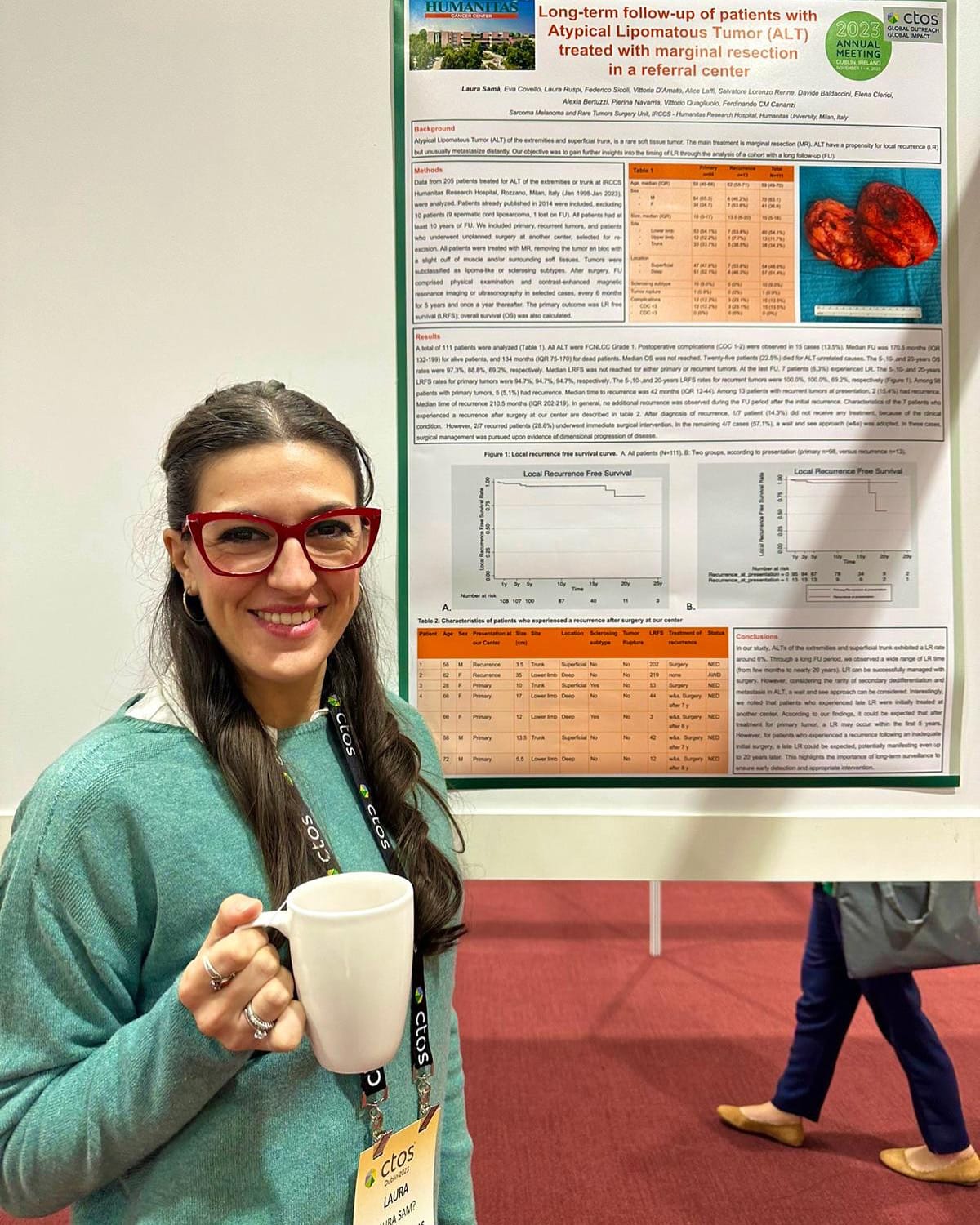
General Surgeon
Sarcoma, Melanoma, and Rare Tumor Surgeon at IRCCS-Humanitas Research Hospital
Rozzano, Italy
"The Surgeon’s Role in Oncology and Patient Care"
I am a surgeon specializing primarily in sarcomas and rare tumors. This means that I constantly face oncology patients with diseases that most have never even heard of. I interact with these patients at various stages. There's the moment of taking their medical history, the moment of communicating the diagnosis, which inevitably leads to the discussion of treatment options. For patients who are candidates for surgery, there's the moment when I explain the type of surgical procedure and its possible consequences. Finally, there are all the questions I see in the eyes of those lying on the operating table, knowing they are about to be anesthetized and that something will have changed when they wake up. In these eyes, you can read a tumult of fears, doubts, questions, anger, resentment, sadness, and euphoria. But you know that despite those eyes, most of the time that face will remain silent. They will just look at you. It is then that I feel I am in a position of maximum listening, not just hearing their stories with my ears but sensing their fears with my heart. This is when I strive to say the right thing, to provide the most comforting answer.
Every patient is an island in an ocean, and the doctor should learn, like a good navigator, to approach each island appropriately, evaluating the seabed, the coast, the inhabitants, and also the conditions of the surrounding sea.
Each of us has, at least once in our life, experienced illness, from a simple, treatable flu to more complex experiences. These are the occasions that make us feel vulnerable and in need of attention, closeness, and reassurance. As a doctor, I have often wondered what the most appropriate attitude is towards patients we encounter.
When I started working as a surgeon, I felt the duty to exercise strong empathy towards the patients I met during my workdays. This often led me to share parts of my own story and to incessantly find common ground with the patient’s story, believing that this could reduce the distance between the patient and the white coat.
Through my ongoing professional development, accumulating daily experience, I have come to realize that the patient, in their fragility and vulnerability, likely seeks not a companion but a steadfast point of support to hold onto when they feel they can't manage alone, when sad thoughts take over.
From that moment on, I used all my strength for my patients not to reduce the gap between two conditions (healthy and sick), but to reduce the gap between two human beings, striving to remain steadfast through my knowledge and professionalism and, above all, to be constantly present.
Medical school curricula need to keep up with the times and innovations in various aspects: clinical, care, scientific, and translational. At the moment, I don't believe that the medical education pathway fully teaches how to understand the experiential and psychological aspects of a patient, especially during moments of physical and psychological suffering. On the other hand, I’m not entirely convinced that it’s solely the responsibility of the University. Those who enter medical school are certainly driven by motivations that are and should remain personal. Among these, however, there should already be an awareness that becoming a doctor inevitably means becoming part of people’s lives.
Medicine is perhaps the profession that, in the most delicate way, involves a constant interpersonal relationship. From the beginning of their studies, students should recognize this role within themselves. Of course, the years of study, but especially the time spent in hospitals, can help this awareness grow, refine, or, conversely, fade away. The university can certainly play a role in this, but in my opinion, more than teaching, we are talking about sensitizing and guiding an attitude.